·
Ulcerative
colitis is an inflammation of the large intestine (colon).
·
The cause
of ulcerative colitis is unknown.
·
Intermittent
rectal bleeding, crampy abdominal pain and diarrhea
often are symptoms of ulcerative colitis.
·
The
diagnosis of ulcerative colitis can be made with a barium enema, but direct visualization
(sigmoidoscopy or colonoscopy) is the most accurate means of
diagnosis.
·
Long-standing
ulcerative colitis is a risk factor for colon cancer.
·
Treatment
of ulcerative colitis may involve both medications and surgery.
·
Ulcerative
colitis also can cause inflammation in joints, spine, skin, eyes, and the liver and its bile ducts.
Ulcerative colitis is a chronic inflammation of the
large intestine (colon). The colon is the part of the digestive system where
water is removed from undigested material, and the remaining waste material is
stored. The rectum is the end of the colon adjacent to the anus. In patients
with ulcerative colitis, ulcers and inflammation of the inner lining of the
colon lead to symptoms of abdominal pain, diarrhea, and rectal bleeding.
Ulcerative colitis is closely related to another
condition of inflammation of the intestines called Crohn's disease. Together, they are
frequently referred to as inflammatory bowel disease (IBD).
Ulcerative colitis and Crohn's diseases are chronic conditions that can last
years to decades. Men and women are affected equally. They most commonly begin
during adolescence and early adulthood, but they also can begin during
childhood and later in life.
It is found worldwide, but is most common in the
United States, England, and northern Europe. It is especially common in people
of Jewish descent. Ulcerative colitis is rarely seen in Eastern Europe, Asia,
and South America, and is rare in the black population. For unknown reasons, an
increased frequency of this condition has been observed recently in developing
nations.
First degree relatives of people with ulcerative
colitis have an increased lifetime risk of developing the disease, but the
overall risk remains small.
Ulcerative
Colitis Diet
There is no clinical or
scientific evidence that supports the theory that a specialized diet may cause
or benefit individuals with ulcerative colitis (UC). However, patients may find
that certain foods aggravate symptoms of ulcerative colitis and they should
avoid such foods. The most common symptoms of ulcerative colitis are rectal
bleeding, abdominal cramping, and diarrhea. Some people recommend avoiding a
high fiber diet (such as raw fruits, vegetables, seeds, nuts, etc.) in addition
to other foods that aggravate symptoms. It may be reasonable to keep a food
journal to track what foods aggravate symptoms and foods that don't aggravate
symptoms (for example, bananas, white rice, white bread, applesauce, bland soft
foods, etc.) Discuss your dietary needs with your treating doctor or a
dietician that specializes in ulcerative colitis and diet
What Causes Ulcerative Colitis?
The cause of ulcerative colitis is not known. To
date, there has been no convincing evidence that it is caused by infection or
is contagious.
Ulcerative colitis likely involves abnormal
activation of the immune system in the intestines. The immune system is
composed of immune cells and the proteins that these cells produce. These cells
and proteins serve to defend the body against harmful bacteria, viruses, fungi,
and other foreign invaders. Activation of the immune system causes inflammation
within the tissues where the activation occurs. (Inflammation is, in fact, an
important mechanism of defense used by the immune system.) Normally, the immune
system is activated only when the body is exposed to harmful invaders. In
patients with ulcerative colitis, however, the immune system is abnormally and
chronically activated in the absence of any known invader. The continued
abnormal activation of the immune system causes chronic inflammation and
ulceration. The susceptibility to abnormal activation of the immune system is
genetically inherited. First degree relatives (brothers, sisters, children, and
parents) of patients with IBD are thus more likely to develop these diseases.
There have been multiple studies using genome wide
association scans investigating genetic susceptibility in ulcerative colitis.
These studies have found there to be approximately 30 genes that might increase
susceptibility to ulcerative colitis including immunoglobulin receptor gene
FCGR2A, 5p15, 2p16, ORMDL3, ECM1, as well as regions on chromosomes 1p36,
12q15, 7q22, 22q13, and IL23R. At this early point in the research, it is still
unclear how these genetic associations will be applied to treating the disease,
but they might have future implications for understanding pathogenesis and
creating new treatments.
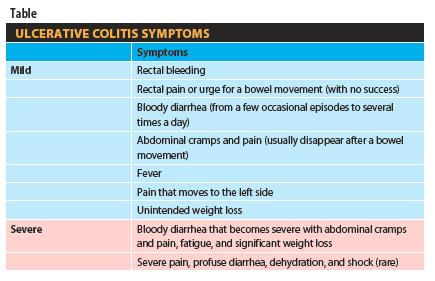
Common symptoms of ulcerative colitis include
rectal bleeding, abdominal pain, and diarrhea, but there is a wide range of
symptoms among patients with this disease. Variability of symptoms reflects
differences in the extent of disease (the amount of the colon and rectum that
are inflamed) and the intensity of inflammation. Generally, patients with
inflammation confined to the rectum and a short segment of the colon adjacent
to the rectum have milder symptoms and a better prognosis than patients with
more widespread inflammation of the colon.
The different types of ulcerative
colitis are classified according to the location and the extent of
inflammation:
1. Ulcerative proctitis refers to inflammation that is limited to the rectum. In many patients
with ulcerative proctitis, mild intermittent rectal bleeding may be the only
symptom. Other patients with more severe rectal inflammation may, in addition,
experience rectal pain, urgency (sudden feeling of
having to defecate and a need to rush to the bathroom for fear of soiling), and
tenesmus (ineffective, painful urge to move one's bowels caused by the inflammation).
2. Proctosigmoiditis involves inflammation of the rectum and the sigmoid colon (a short
segment of the colon contiguous to the rectum). Symptoms of proctosigmoiditis,
like that of proctitis, include rectal bleeding, urgency, and tenesmus. Some
patients with proctosigmoiditis also develop bloody diarrhea and cramps.
3. Left-sided colitis involves inflammation that starts at the rectum and extends up the left
colon (sigmoid colon and descending colon). Symptoms of left-sided colitis
include bloody diarrhea, abdominal cramps, weight loss, and left-sided abdominal pain.
4. Pancolitis or universal colitis refers to inflammation affecting the entire colon
(right colon, left colon, transverse colon and the rectum). Symptoms of
pancolitis include bloody diarrhea, abdominal pain and cramps, weight loss, fatigue,
fever, and night sweats. Some patients with pancolitis
have low-grade inflammation and mild symptoms that respond readily to
medications. Generally, however, patients with pancolitis suffer more severe
disease and are more difficult to treat than those with more limited forms of
ulcerative colitis.
5. Fulminant colitis is a rare but severe form of pancolitis. Patients with fulminant
colitis are extremely ill with dehydration, severe abdominal pain,
protracted diarrhea with bleeding, and even shock.
They are at risk of developing toxic megacolon (marked dilatation of the colon
due to severe inflammation) and colonic rupture (perforation). Patients with
fulminant colitis and toxic megacolon are treated in the hospital with potent
intravenous medications. Unless they respond to treatment promptly, surgical
removal of the diseased colon is necessary to prevent colonic rupture.
While the intensity of colon inflammation in
ulcerative colitis waxes and wanes over time, the location and the extent of
disease in a patient generally stays constant. Therefore, when a patient with ulcerative
proctitis develops a relapse of his or her disease, the inflammation usually is
confined to the rectum. Nevertheless, a small number of patients (less than
10%) with ulcerative proctitis or proctosigmoiditis can later develop more
extensive colitis. Thus, patients who initially only have ulcerative proctitis
can later develop left-sided colitis or even pancolitis.










No comments:
Post a Comment